Aching hips interfere with the everyday life of millions of people, whether it is a walk or proper sleep. Being an orthopedic physician with a long-term history of experience, the recurrent discomfort is a sign of underlying structural problems and not of muscle tension. This is a complete guide to bring out the real causes, course, diagnoses, and evidence-based treatment.
Osteoarthritis: Wear and Tear Culmination
Osteoarthritis is the most common source of pain, and the cartilage of the hip joints is degenerated after decades of usage. The elderly patients over 50 years old, who are mostly obese and those with a prior experience of any injury, complain of deep groin pain, which intensifies during weight-bearing activities like climbing the stairs and getting out of the chair.
It is the fact that it has morning stiffness that is less than 30 minutes, and this is what distinguishes it from inflammatory arthritis. X-rays reveal that the joint space is narrow, osteophytes are present, and there is subchondral sclerosis.
The initial management involves weight loss, physiotherapy on the gluteal muscles, and intra-articular hyaluronic acid injection or PRP. Hip replacement surgery in Mumbai is required when the end-stage disease is advanced, and the hip surgery will restore almost normal functioning, with 98 percent satisfaction of the patients.
Avascular Necrosis: Bone Death from Vascular Compromise
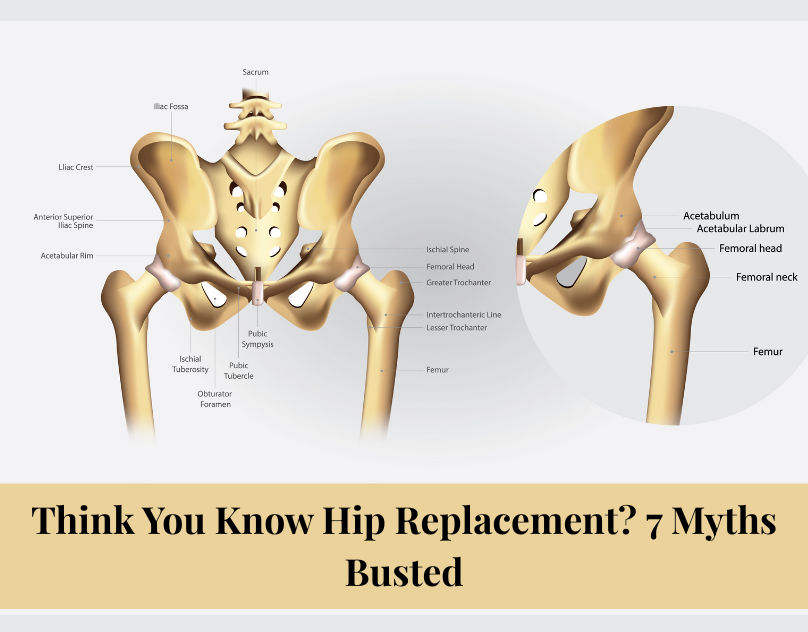
AVN happens where the blood supply to the femoral head ceases to be adequate, normally through sustained corticosteroid use, persistent alcoholism, or other overall illnesses like sickle cell anemia. Stage 2, which is initially asymptomatic, makes the night pains not relieved by rest; Stage 3 results in antalgic gait and restriction of rotation. MRI gives a final diagnosis of a collapsed femoral head.
In early cases, core decompression using bone grafting delays the course by 60%. Stage 4 cannot be reversed, and it involves hip replacement surgery to ensure painless movement in Mumbai.
Greater Trochanteric Syndrome: Side Hip Pain
GTPS entails trochanteric bursitis, gluteal tendinopathy, and external snapping hip. Middle-aged women are the most affected by repetitive hip abduction stresses, such as climbing or sleeping on the affected side. Lateral sharp pain moves to the thigh and is made worse by one-leg positioning.
Ultrasound is dynamic in proving the presence of fluid or tendon tears. Eccentric strengthening, shockwave therapy, and injection of corticosteroids with the help of fluoroscopy can result in a 80% success rate of conservative treatment. Endoscopic bursectomy is useful in refractory cases.
Femoral acetabular impaction and Labral Pathology
FAI (cam or pincer variations) and labral tears in the acetabulum are the bane of young active adults, which results in mechanical groin pain when deeply flexed or rotated. There is pathology in clicking and catching during squatting. In case of lumbar problems, hip-spine syndrome makes it difficult to diagnose.
The 3T MR arthrography can visualize labral defects and an alpha angle greater than 55. Arthroscopic labral repair using femoroplasty demonstrates 85-90% return to sport in 6 months, and is thus longer lasting than conservative care.
Inflammatory Arthropathies: Systemic Joint Assault
Rheumatoid arthritis and ankylosing spondylitis attack the synovial lining, resulting in bilateral morning stiffness, which is greater than 1 hour and change in buttock pain. Increased ESR/CRP and positive HLA-B27 are confirmatory. DMADs and biologics such as adalimumab reduce advances in 70 percent.
Stress Fractures and Occult Injuries
Femoral neck stress fractures occur in runners and military recruits due to recurrent loading, as manifested by insidious pain in the groin, aggravated at night. The Hop test reproduces symptoms.
The MRI identifies the presence of bone marrow edema earlier than X-ray alterations. The non-operative method of healing has a 20% chance of displacement; the prophylaxis screw fixation is safer. Insufficiency fractures plague osteoporotic older adults who have had minor trauma.
Lumbar Spinal and Pelvis Referred Pain
The pain is referred through the sciatic and obturator nerves as L5-S1 disc herniation or sacroiliac dysfunction. A positive straight-leg test and the FABER test distinguish spinal origin. MRI is a must for lumbar spine radiculopathy solution, which solves 75% of the cases that had been misdiagnosed as hip pain. Piriformis syndrome traps the sciatic muscle and is similar to that of the hips.
Septic Arthritis and Neoplastic Causes
Septic hip is infrequent but devastating and is characterized by fever, chills, and acute weight-bearing deficiency. Aspiration yields >50,000 WBCs/μL. Emergency debridement averts the destruction of the joints. Diffuse bone pain at night that is not relieved with analgesics is a sign of metastatic bone disease or primary chondrosarcoma- biopsy obligatory.
Planned Diagnostic Process
- Step 1: Detailed history- pain location (groin= intra-articular and lateral= extra-articular), night pains, trauma, and systemic symptoms.
- Step 2: Physical exam- log roll to examine effusion, FADIR to examine FAI, Trendelenburg to examine abductor weakness.
- Step 3: Imaging sequence- AP pelvis X-ray, MRI of hips/ spine, and DEXA to exclude osteoporosis.
- Step 4: Labs- CBC, ESR/CRP, RF, and HLA-B27 panel.
| Condition | Hallmark Symptom | Diagnostic Test | Primary Treatment |
| Osteoarthritis | Groin ache stairs | X-ray narrowing | Physio → Hip replacement surgery in Mumbai |
| AVN | Night pain limp | MRI femoral collapse | Core decompression → THR |
| GTPS | Lateral tenderness | Ultrasound | ESWT → Injection |
| Labral Tear/FAI | Mechanical catching | MR arthrogram | Hip arthroscopy |
| Inflammatory | Prolonged stiffness | HLA-B27 positive | DMARDs/biologics |
| Stress Fracture | Exercise night pain | MRI marrow edema | Rest → ORIF |
| Referred Spine | Buttock radiation | Lumbar MRI | Spinal intervention |
Red Flags that need to be evaluated urgently
- Sudden severe pain post-fall
- Development of night pain despite rest.
- Symptoms of the constitution (fever, loss of weight)
- The abrupt constriction of the blood vessels of the brain.
Once it occurs, an orthopedic physician in Thane must be called; the first and most important step to eliminate disastrous outcomes is the quickness of the treatment.
Conservative Treatment Ladder (90% Success)
- Lifestyle: BMI loss (10% weight loss decreases pain by a half)
- Drugs: NSAIDs, acetaminophen, duloxetine as the neuropathic component.
- More Injections: PRP is better in the long run than ultrasound-guided corticosteroids.
- Rehabilitation: Gait training, glute medius isometrics, aquatic therapy.
- Advanced: ESWT, platelet-rich plasma is better than steroids after 2 years.
Operative Treatment of Failed Conservatism.
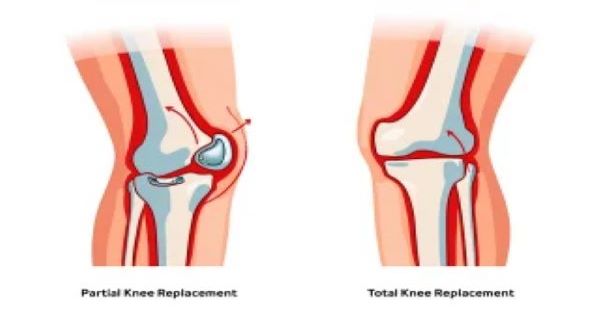
Labrum/FAI (85% success) is repaired by arthroscopy. OSAVN can be treated by end-stage hip replacement in Mumbai; the hip replacement has a 99% 15-year survival with ceramic bearings. Robotic aid increases accuracy with dysplastic hips.
Prevention Through Smart Habits
- Keep a good body weight, Vitamin D 2000IU a day, so that the bones are healthy.
- Balance/proprioception training decreases falls by 40%.
- An ergonomic workstation avoids repetitive strain.
Conclusion
Relentless pain in the hip requires systematic enquiry – self-resolution is uncommon. Disability is conceived through procrastination; it is disability that is caused by early diagnosis. Engage qualified experts for the best results.
Don’t let hip pain control you. Get access to high-level diagnostics and individualized treatment regimens with Team Ortho Robotics in the Kaushalya Medical Foundation Hospital- book your whole hip pain check-up now!
FAQs
1. When should hip replacement surgery be performed in Mumbai?
End-stage OA/AVN with unsuccessful conservative care; only in 98 percent of cases a restoration of functions.
2. What is the diagnosis of an orthopedic doctor in Thane to determine the origin of the hip pain?
History, FADIR exam, X-ray/MRI sequence is accurate in localizing OA vs. labral tears.
3. Is it possible that chronic hip pain can be solved without surgery?
Yes, 90% are getting better with physio/injections; structural failure only surgery.